What Are the Side Effects of Taking Contraceptive Pills for Women with Pcos?
HiherbsOfficial
Share
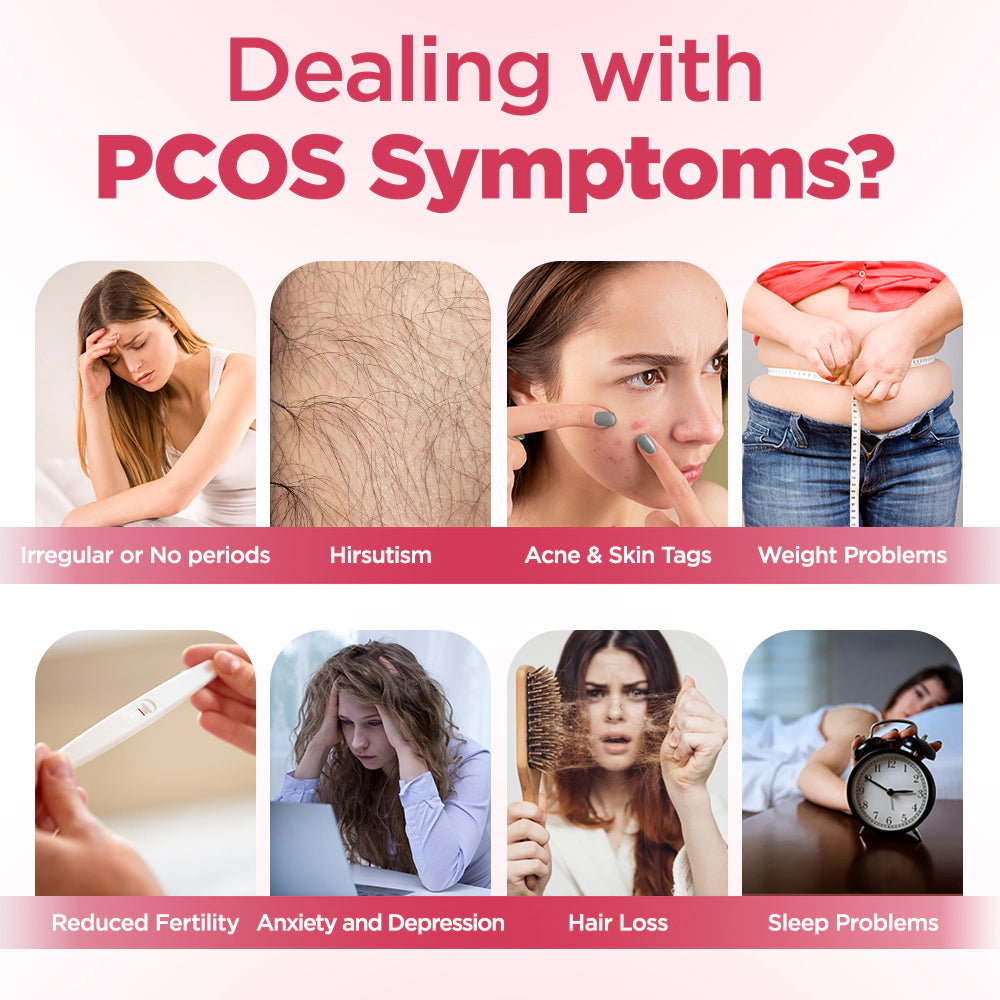
For decades, synthetic hormones like birth control pills have been the go-to solution for managing Pcos symptoms. Doctors often prescribe them to regulate menstrual cycles, reduce acne, and lower androgen levels. On the surface, they seem like a miracle fix—quick, accessible, and backed by decades of medical use. But beneath this veneer of convenience lies a troubling reality: synthetic hormones often merely mask the symptoms and do not truly address the underlying issue. Moreover, they can also cause new and long-term health problems.
A paper published in the Journal of Clinical Endocrinology and Metabolism in 2023 showed that up to 40% of PCOS (Polycystic Ovary Syndrome) female patients could not tolerate the side effects of contraceptive pills, and thus stopped using hormonal contraceptives within two years. Reddit is filled with stories like that of 28-year-old Sarah, who shared: "My acne improved in the second month, but by the third month, my pimples started to flare up severely again." These reports raise a key question: Synthetic hormones cannot cure PCOS; they merely put the symptoms on hold. Stopping the medication or over time, side effects will follow.

Sarah's original post on reddit
What's worse is that synthetic hormones can disrupt the hypothalamic-pituitary-ovarian (HPO) axis, which is a feedback loop that controls ovulation and metabolic health and involves delicate hormones. Birth control pills disrupt this system, and over time, it will exacerbate insulin resistance, which is the fundamental cause of PCOS. This forms a vicious cycle where women rely on the drugs, but these drugs actually aggravate the condition that they are supposed to treat.

HPO
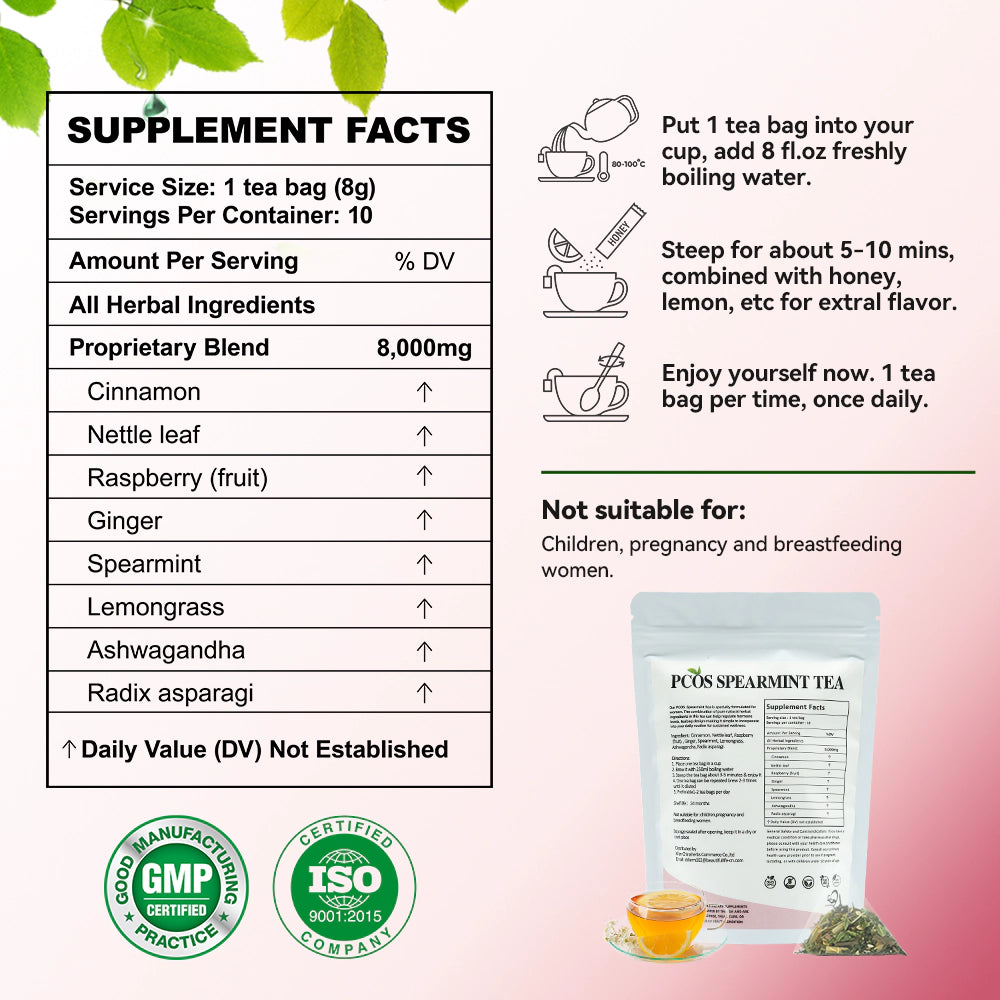
Tip: For women seeking a permanent cure for this condition, plant-based alternatives like spearmint tea that can naturally regulate hormone levels are more suitable for them.
Weight Gain
One of the most devastating side effects of synthetic hormones is unexplained weight gain—a cruel irony for women already struggling with PCOS-related metabolic issues. Birth control pills containing progestins like levonorgestrel can increase appetite, fluid retention, and fat storage, particularly around the abdomen. A 2023 meta-analysis in Diabetes Care found that women using hormonal contraceptives had a 14% higher risk of developing insulin resistance compared to non-users, directly fueling PCOS progression.
Synthetic progestins bind to glucocorticoid receptors, which regulate metabolism and stress responses. This interaction can spike cortisol levels, triggering cravings for sugary, high-carb foods. Over time, this dysregulates blood sugar and amplifies androgen production, worsening hirsutism and acne. As one user on r/PCOS lamented, “I gained 30 pounds on the pill, and my doctor just shrugged and said, ‘It’s common.’ But no one warned me it would make my PCOS harder to manage.”
Extremely Emotional Fluctuations
While synthetic hormones may temporarily ease physical PCOS symptoms, they often unleash chaos on mental health. Birth control pills alter neurotransmitter activity in the brain, particularly serotonin and dopamine—key regulators of mood. A 2023 study in Psychoneuroendocrinology found that women using hormonal contraceptives had a 23% higher risk of depression compared to non-users. For PCOS patients already prone to anxiety due to hormonal imbalances, this can feel like adding fuel to a fire.
Reddit threads like “Birth Control Ruined My Mental Health” are filled with harrowing stories. Jessica, a 25-year-old with PCOS, shared: “After six months on the pill, I started having panic attacks and felt like I didn’t recognize myself. My doctor said it was ‘just stress,’ but going off the pills was the only thing that helped.” Such testimonials underscore how synthetic hormones can destabilize the hypothalamic-pituitary-adrenal (HPA) axis, the body’s stress-response system, leading to chronic anxiety and emotional numbness.
Ashwagandha provide a gentler alternative. Ashwagandha has been shown in clinical trials to reduce cortisol levels by 28% and improve emotional resilience in PCOS patients. Unlike synthetic hormones, which blunt the body’s natural feedback loops, ashwagandha supports the HPA axis without overriding it—a crucial distinction for long-term mental health.
Risk of Infertility
Many women with PCOS take contraceptive pills to "regulate" their menstrual cycles, but later they found that this method had no effect on improving fertility. Synthetic hormones can inhibit ovulation and cause artificial bleeding that mimics a normal menstrual cycle. An article in the journal Human Reproduction in 2023 clearly stated that long-term use of contraceptive pills can lead to a decrease in anti-Müllerian hormone (AMH) levels, which is a key indicator of ovarian reserve, and this also reflects that the ovaries of some patients have aged at an accelerated rate.
Take Maria’s story: After using birth pills for eight years, she struggled to conceive for three years post-discontinuation. Tests showed her AMH levels had dropped to 0.8 ng/mL (normal for her age: 1.5–4.0). “I wish I’d known the pill was just putting a Band-Aid on the problem,” she said. Cases like hers expose the harsh truth: synthetic hormones silence PCOS symptoms but allow underlying issues like insulin resistance and inflammation to fester unchecked.
The Rebound Effect: When Treatment Ends
Quitting synthetic hormones often feels like stepping off a cliff. The “rebound effect”—where PCOS symptoms return with greater severity—is a well-documented phenomenon. A 2022 study in Clinical Endocrinology found that 68% of women experienced worsened acne, hair loss, and irregular cycles within six months of stopping birth control. This occurs because synthetic hormones suppress the body’s natural hormone production; when removed, the system struggles to recalibrate.
Natural therapy focuses on gradual and sustainable treatment. For instance, green tea or chamomile can restore ovulation function by improving insulin sensitivity. Unlike the sudden changes in hormone levels caused by contraceptive pills, these therapies follow the body's physiological rhythm and generally do not have rebound risks.
The Financial and Emotional Toll
In the United States, the average annual cost for each person for hormonal contraception exceeds $600. This does not include the cost of medical visits or the expenses for managing side effects such as weight gain. For patients with polycystic ovary syndrome (PCOS), this economic pressure further exacerbates their emotional burden of being trapped in a cycle of ineffective treatment.
Communities like Reddit/PCOS thrive because women crave alternatives. One user wrote: “I spent thousands on birth control and metformin, but only saw real change after switching to PCOS Tea long-term results Reddit users recommended.” These stories highlight a shift toward affordable, holistic solutions that prioritize body autonomy over pharmaceutical dependency.
Conclusion
The journey of managing PCOS is fraught with contradictions, treatments that promise relief but deliver new burdens, quick fixes that deepen long-term struggles, and a medical system that often prioritizes suppression over healing. Synthetic hormones epitomize this paradox. While they may offer temporary symptom control, their legacy weight gain, emotional turmoil, fertility illusions, and financial strain, leaves many women feeling betrayed by the very system meant to help them.
A growing body of research and grassroots advocacy is shifting the narrative. Studies now confirm what women have long suspected: PCOS is not a life sentence of dependency on synthetic drugs. The hypothalamic-pituitary-ovarian axis is remarkably resilient; when supported through targeted nutrition, stress reduction, and botanicals, it can recalibrate naturally. For instance, spearmint tea—a staple in PCOS Tea ingredients decoded—has been shown in randomized trials to reduce free testosterone by 30% within 30 days, rivaling pharmaceutical interventions without the side effects.
This isn’t about rejecting modern medicine but embracing a hybrid approach. Tools like natural hormone regulation and cycle-tracking apps empower women to collaborate with their bodies rather than fight against them. As one Reddit user summarized: “I used to think birth control was my only option. Now I’m learning to listen to my body and it’s telling me to heal, not hide.”
The road ahead may require patience, unlike synthetic hormones, natural solutions work gradually, but the destination is worth it: true hormonal harmony, fertility on your terms, and a body that feels like an ally, not a battleground.