3 Silent Signs of PCOS: Could Your Hormones Be Out of Balance?
HiherbsOfficial
Share
Catalogs:
Overview
Polycystic Ovary Syndrome (PCOS) is the most common hormonal disorder among women of reproductive age, yet its complexity often leaves both patients and doctors puzzled. According to the World Health Organization (2023), 1 in 10 women globally are affected by PCOS, with nearly 70% remaining undiagnosed. This condition goes far beyond "irregular periods" or "fertility struggles"—it revolves around a chain reaction of hormonal imbalances, particularly elevated androgens (like testosterone) and insulin resistance.
Emerging research offers hope: natural ingredients like ashwagandha and lifestyle interventions may provide novel solutions. A 2022 double-blind trial in Phytomedicine found that women taking ashwagandha extract for 12 weeks experienced an average 18% reduction in testosterone levels. But first, we must decode the silent signals our bodies send.
The Basics of PCOS
PCOS is diagnosed using the 2003 Rotterdam Criteria, requiring at least two of the following:
1. Oligo-ovulation: Fewer than 8 menstrual cycles per year or cycles longer than 35 days.
2. Hyperandrogenism: Confirmed via blood tests or symptoms like hirsutism or severe acne.
3. Polycystic Ovaries: Presence of 12+ follicles (2-9 mm in diameter) per ovary on ultrasound.
However, PCOS is fundamentally a vicious cycle of metabolism and hormones. High androgens suppress follicle development, causing anovulation, while insulin resistance promotes fat storage, further stimulating ovarian androgen production. A 2021 Journal of Clinical Endocrinology study found that 58% of PCOS patients have significant insulin resistance, explaining why many struggle with weight loss despite dietary efforts.
The key to managing PCOS lies in breaking this cycle. While medications (like birth control pills or metformin) are standard, more women are turning to natural approaches for hormone balance, such as:
· Adaptogens (e.g., ashwagandha) to lower stress hormones like cortisol.
· Omega-3 fatty acids to improve insulin sensitivity.
3 Silent Signs of PCOS – Androgen-Related Symptoms
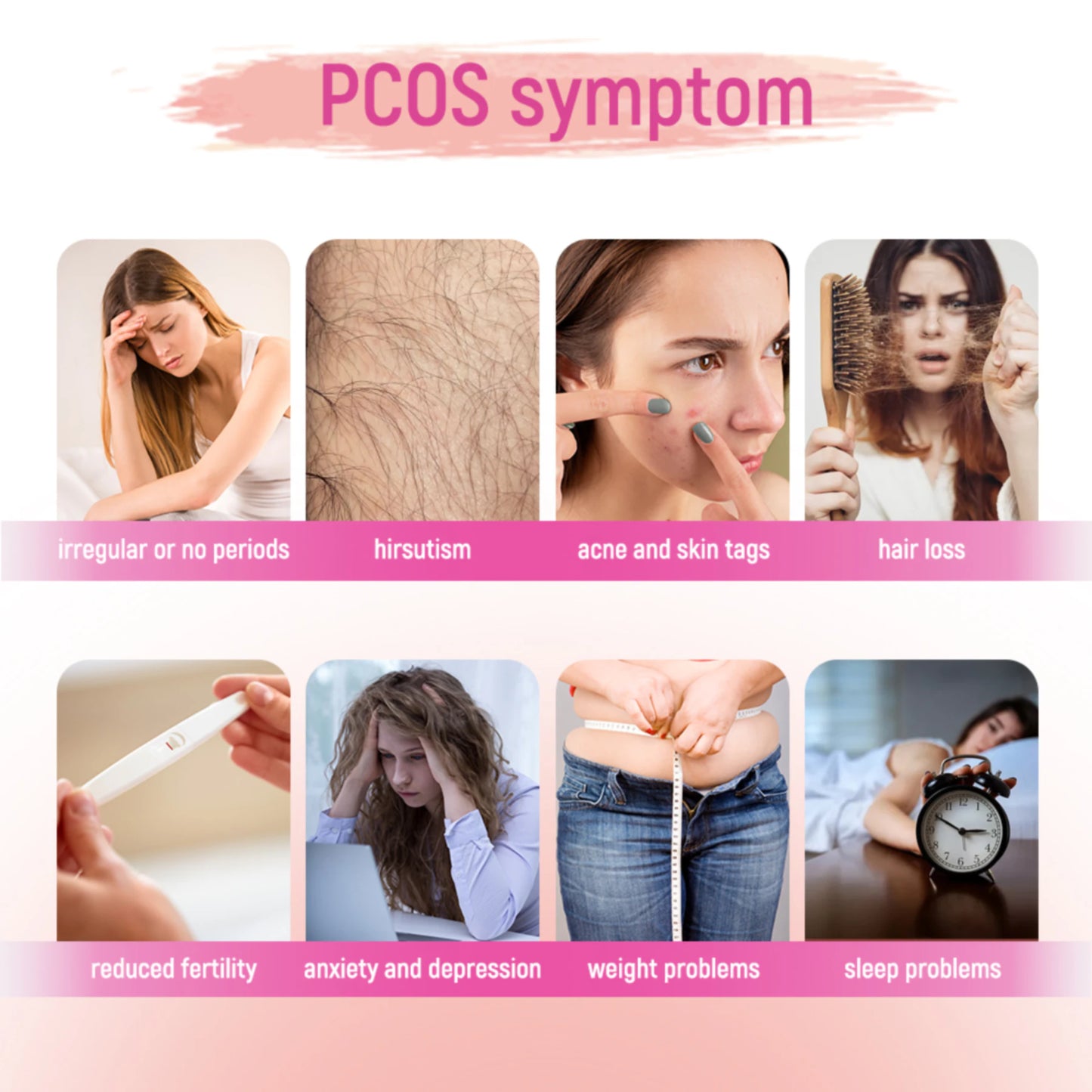
Hirsutism: Unwanted Hair Growth

When androgens like testosterone are elevated, women may develop coarse hair in typically male-pattern areas—such as the upper lip, chin, chest, or lower abdomen. Clinicians use the Ferriman-Gallwey Scoring System to assess severity: 9 body areas are rated for hair density, with a total score ≥8 indicating hyperandrogenism. A 2021 Journal of Clinical Endocrinology & Metabolism study found that 70% of PCOS women score above 8, and hirsutism correlates with insulin resistance severity.
Ethnic variations matter. For example, East Asian women might see sparse terminal hair on the chin or around nipples, while South Asian or Middle Eastern women often experience more pronounced growth. In natural therapies, ashwagandha has shown potential in animal studies to reduce free testosterone, though human trials remain limited.
Stubborn Acne: Hormonal Skin Alerts
Deep, cystic acne along the jawline, neck, or back often acts as a "skin signature" of high androgens. Unlike teenage acne, these breakouts flare cyclically, worsening pre-menstrually. A 2022 Journal of Investigative Dermatology study noted that 45% of PCOS patients continue experiencing inflammatory acne beyond age 30, with poor response to topical treatments like benzoyl peroxide.
Androgens worsen acne by boosting sebum production and follicle keratinization. Intriguingly, natural ingredients like spearmint show promise: a 2020 clinical trial found that women drinking 2 cups of spearmint tea daily for 6 weeks saw a 25% drop in testosterone and 30% less severe acne.
Thinning Hair: The Burden of Androgenic Alopecia
When testosterone converts to dihydrotestosterone (DHT), it attacks hair follicles, leading to gradual thinning. PCOS-related hair loss typically follows a receding hairline or diffuse thinning at the crown ("Christmas tree pattern"). A 2023 International Journal of Dermatology survey revealed that 40% of PCOS women initially blamed their hair loss on stress or poor nutrition.
Clinicians may use the Ludwig Scale to grade severity. In natural interventions, topical rosemary oil has shown hair-regrowth effects comparable to minoxidil in small studies, though its mechanisms remain unclear.
Natural Diagnostic Indicators for PCOS
Irregular Cycles: Your Body’s Silent SOS
Menstrual cycles act as a “barometer” of hormonal health. For PCOS patients, cycles longer than 35 days or fewer than 8 periods per year are red flags. A 2023 Human Reproduction study found that 82% of women with cycles >35 days have high androgens or insulin resistance. Alarmingly, chronic irregularities (e.g., no periods for 3+ months) increase risks of endometrial hyperplasia or cancer.
Self-tracking tools:
· Menstrual cycle template: Log dates, flow intensity, and symptoms (e.g., cramps or mood swings).
· Warning signs: Sudden cycle changes (±7 days) may signal hormonal shifts.
Health risks of irregular cycles→Why Birth Control Pills Worsen PCOS Symptoms
Skin & Hair Changes: Androgens’ Visible Proof
Beyond hirsutism and acne, high androgens can trigger:
· Androgenic alopecia: Thinning hair and receding temples.
· Acanthosis nigricans: Dark, velvety patches in skin folds, strongly linked to insulin resistance.

Acanthosis nigricans
A 2022 Journal of Clinical Dermatology study found that 91% of women with both acne and acanthosis nigricans are diagnosed with PCOS. For self-checks, monthly photos of skin and scalp under consistent lighting can reveal subtle changes.
Understanding Hormonal Imbalances in Women
Testosterone: Normal vs. Dangerous Levels
Normal total testosterone levels in women range from 0.2-0.8 ng/mL (blood test). Levels above 0.8 ng/mL sharply increase anovulation risks. A 2023 Fertility and Sterility study showed that each 0.1 ng/mL rise in testosterone raises the chance of missed ovulation by 15%. High androgens also disrupt metabolism via:
· Visceral fat storage: Waist-to-hip ratio >0.85.
· Insulin resistance: Fasting insulin >10 μIU/mL.
The Domino Effect of Hormonal Chaos
Hyperandrogenism and insulin resistance form a vicious cycle: insulin prompts ovaries to produce more testosterone, which worsens insulin resistance. A 2021 Endocrine Reviews paper noted that PCOS women face a 4x higher diabetes risk. Additionally, stress-induced cortisol spikes elevate free testosterone, worsening hair loss and anxiety.
Could Your Hormones Be Out of Balance? – The Link to PCOS
Hormone Testing: From Labs to Home Kits
To confirm hormonal imbalances, doctors typically recommend:
1. Blood Tests:
· LH/FSH Ratio: A normal ratio is ~1:1. In PCOS, LH/FSH often exceeds 2:1, even reaching 3:1 (Reproductive Biology, 2022).
· Free Testosterone: Reflects active androgen levels (normal: 0.2-0.8 ng/mL).
2. Saliva Hormone Tests: Track cortisol and free testosterone fluctuations. Home kits (e.g., EverlyWell) show 85% correlation with lab results (Journal of Family Medicine, 2023).
Self-monitoring tools:
· Cycle Apps: Flo or Clue analyze menstrual patterns and symptom trends.
· Symptom Diary: Log weight, hair changes, and mood swings for 3 months to identify patterns.
Pro Tip: Avoid birth control pills or hormone supplements for 1 month before testing.
Natural Approaches to Self-Diagnose PCOS
Symptom Tracking: Be Your Own Health Detective
Track these metrics for 3 months:
· Menstrual Cycles: Note dates, flow (light/moderate/heavy), and symptoms (e.g., breast tenderness).
· Skin & Hair: Monthly photos of face, back, and scalp to compare changes.
· Weight & Waist: Weekly measurements to calculate waist-to-hip ratio (>0.85 is abnormal).
A 2023 Nature Medicine study found that women who track symptoms reduce diagnosis time by 6 months.
Diet & Stress: Silent Hormone Modulators
· Low-GI Diet: Swap white rice for brown rice and choose whole-grain bread. A 2021 Nutrition trial showed low-GI diets reduce testosterone by 12% in PCOS women.
· Anti-inflammatory Foods: Omega-3-rich salmon, flaxseeds, and walnuts curb androgen production.
· Stress Reduction: Daily 10-minute meditation or yoga lowers cortisol. A 2022 Journal of Stress Research study found that every 10% drop in cortisol reduces free testosterone by 0.15 ng/mL.
· Natural Allies: Drinking 2 cups of spearmint tea daily may slash testosterone by 25% —[Explore how spearmint regulates hormones→Spearmint Tea and Androgen Reduction Study].
Summary
Managing PCOS is a marathon, not a sprint. While medical interventions are crucial, natural strategies (e.g., adaptogens, dietary tweaks) offer sustainable support. Ingredients like ashwagandha and spearmint—backed by early research—will be explored in-depth in future articles.
Remember, your body is sending signals. Learning to listen is the first step toward healing.